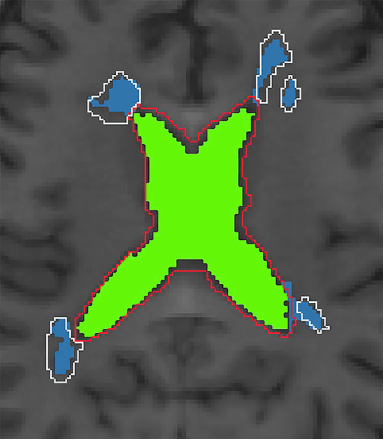
We investigated how chronic inflammatory lesions in multiple sclerosis evolve over time by studying their expansion patterns and relationship to disease progression in patients with relapsing-remitting MS over a 4-year period.
Key Findings:
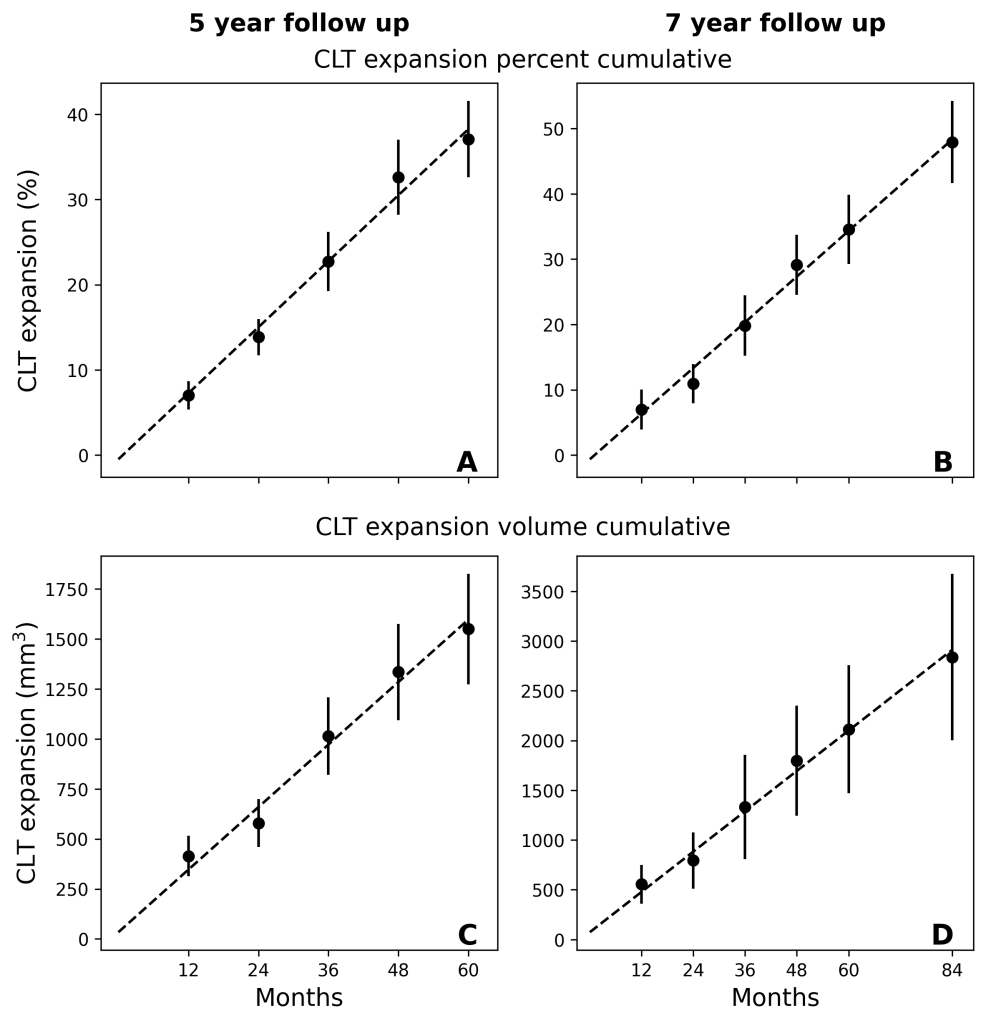
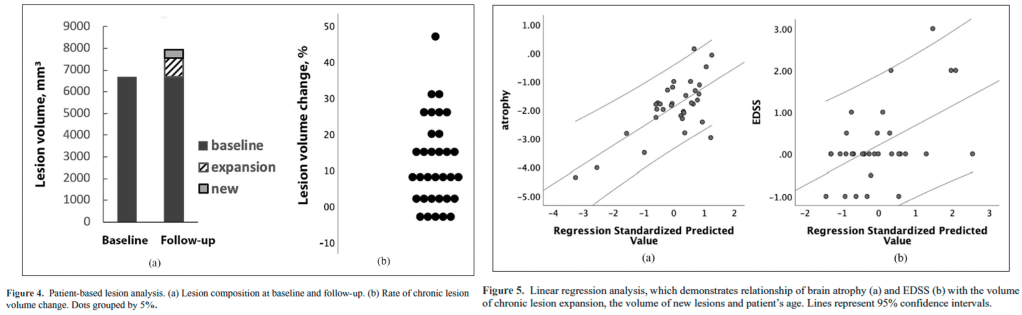
- The expansion of chronic lesions, rather than formation of new lesions, accounts for most (67%) of total brain lesion volume increase in MS patients
- Nearly half (46%) of chronic lesions showed significant expansion, while only 12% shrank over time
- Lesion expansion strongly correlated with both brain atrophy and increased disability, suggesting it drives disease progression
- Older patients showed higher rates of lesion expansion, potentially explaining accelerated disability in aging MS patients
Novel Technical Advances:
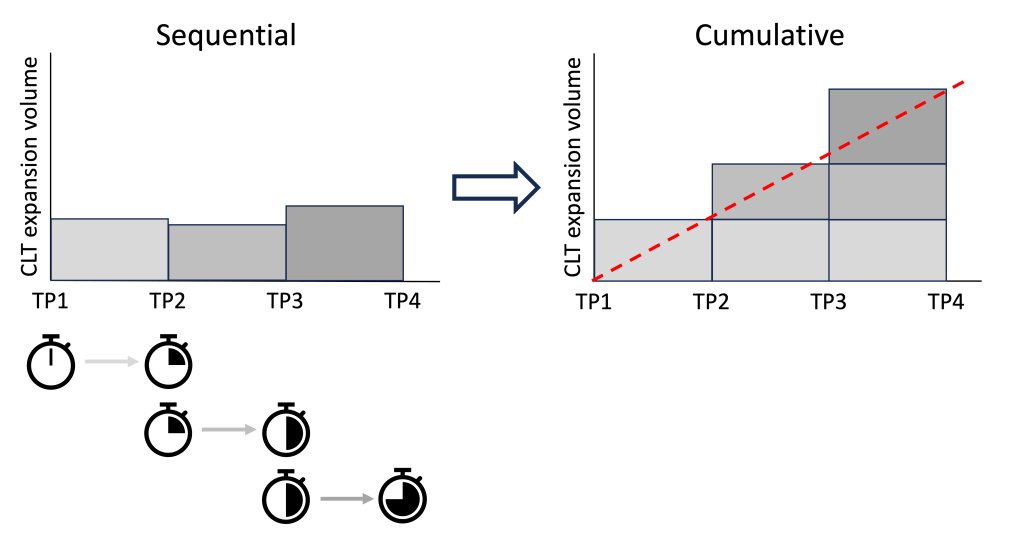
- Developed sophisticated imaging analysis methods to precisely track individual lesion changes over time
- Created automated algorithms to distinguish between expanding chronic lesions and new lesion formation
- Established quantitative measures to assess tissue damage within expanding lesions using diffusion imaging
- Implemented rigorous controls for brain atrophy effects on lesion measurements
Clinical Implications:
- The dominant role of chronic lesion expansion in disease progression suggests new therapeutic targets are needed
- Treatments focusing only on preventing new lesions may not adequately address ongoing tissue damage
- Monitoring chronic lesion expansion could help identify patients at higher risk of progression
- Age-related increases in lesion expansion indicate older patients may need different therapeutic approaches
Why It Matters:
This study fundamentally changes our understanding of how MS progresses by showing that the slow expansion of existing lesions, rather than formation of new ones, is the primary driver of accumulating disability. This challenges the traditional focus on preventing new lesion formation and suggests that therapies targeting chronic inflammation at lesion edges could help prevent disease progression. The findings explain why current treatments, while effective at reducing new lesions, may not fully prevent advancing disability, especially in older patients. This work provides crucial evidence for developing new therapeutic strategies aimed at the smoldering inflammation that causes lesion expansion.