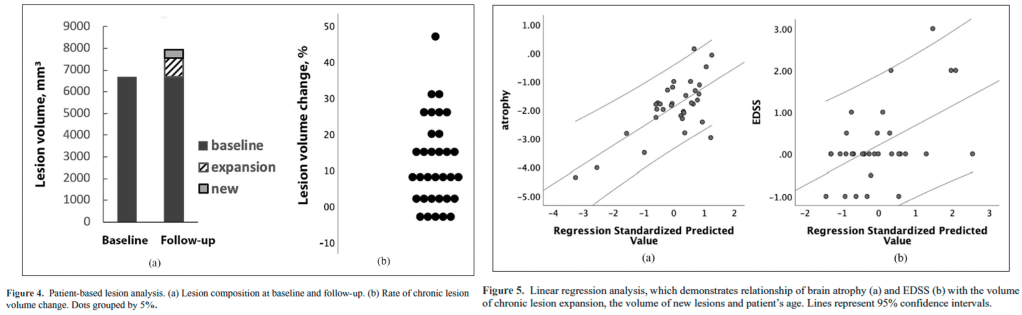
Progressive Tissue Loss in Chronic MS Lesions: Mechanisms of Brain Volume Loss
This longitudinal study reveals how ongoing tissue damage within chronic MS lesions contributes to brain atrophy, offering new insights into disease progression even in treated patients.
Key Findings:
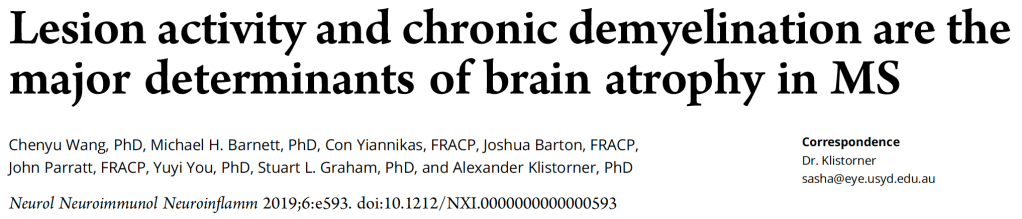
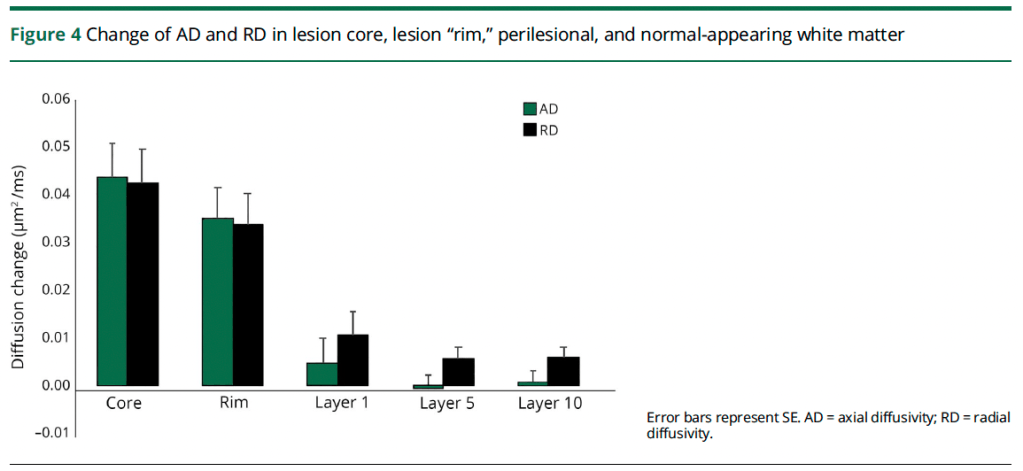
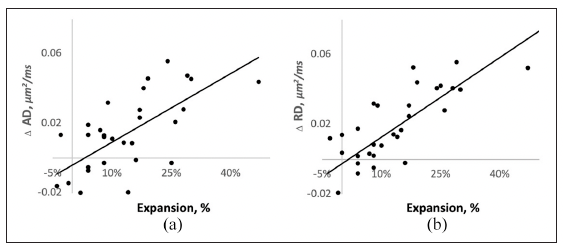
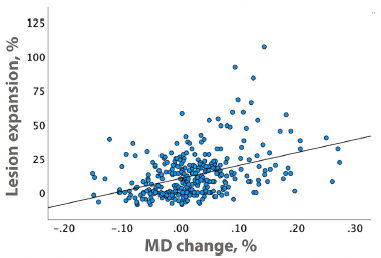
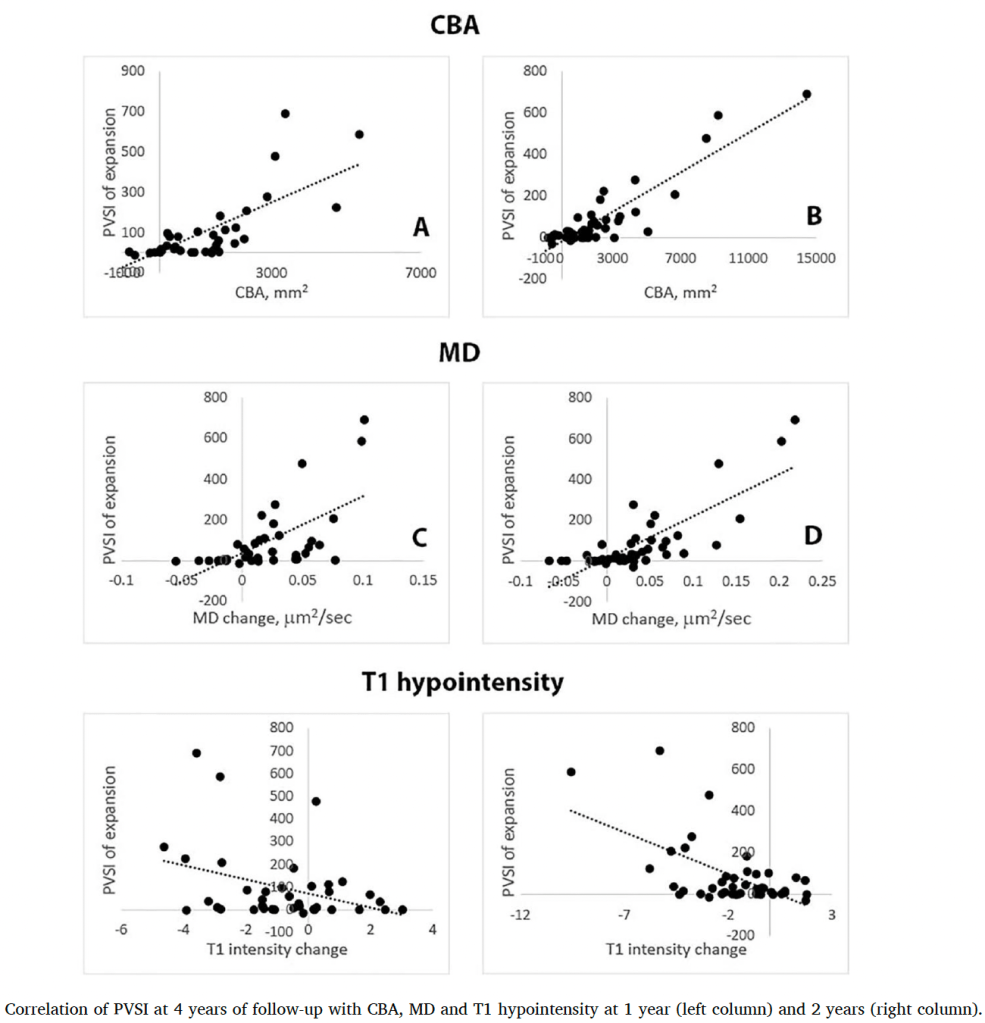
- Significant tissue loss occurs within chronic inactive MS lesions, with water diffusion increasing by 3.3% annually in lesion cores
- Brain volume decreased by approximately 2% over the 5-year study period, showing continued atrophy despite treatment
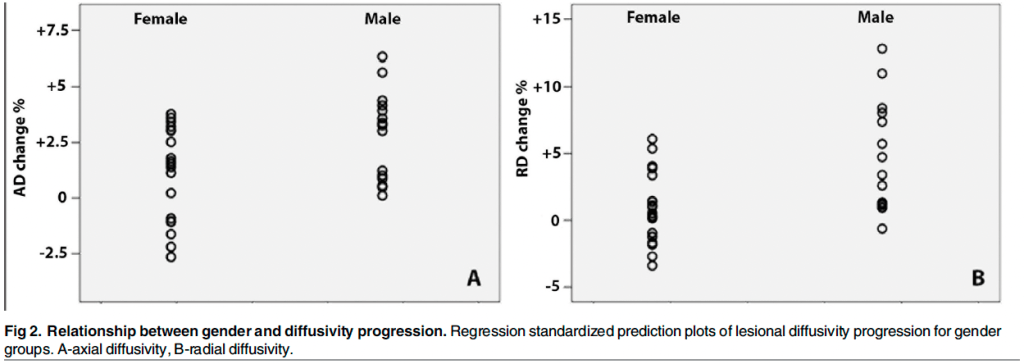
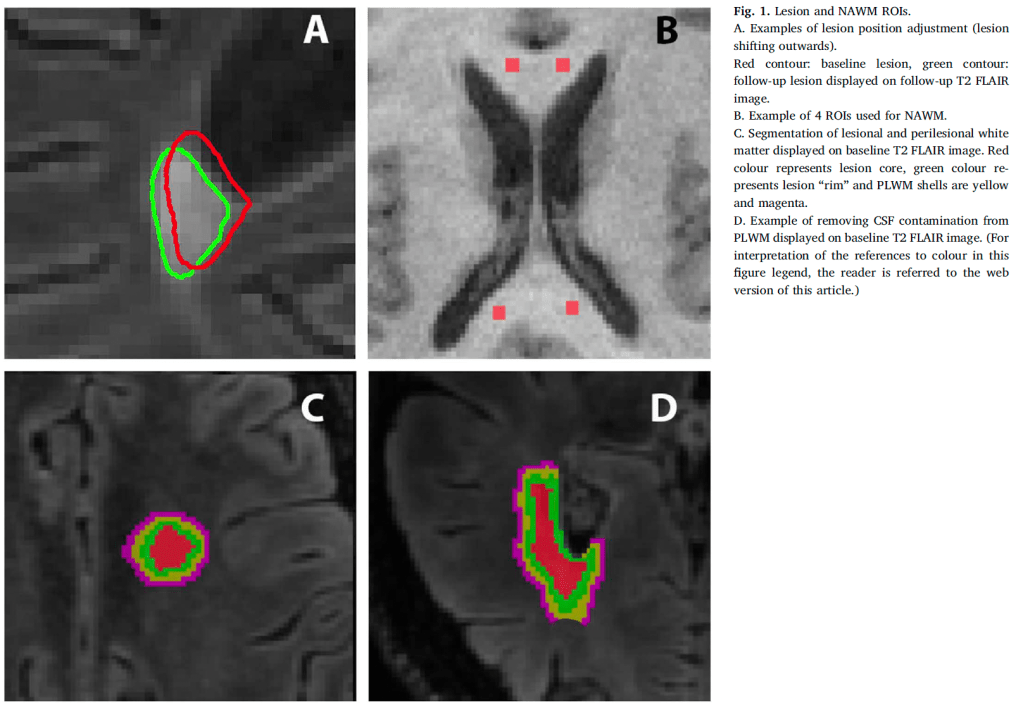
- Males showed nearly twice the rate of tissue damage compared to females, suggesting important gender differences in disease progression
- Tissue damage within chronic lesions strongly correlated with overall brain atrophy, explaining 38% of brain volume changes
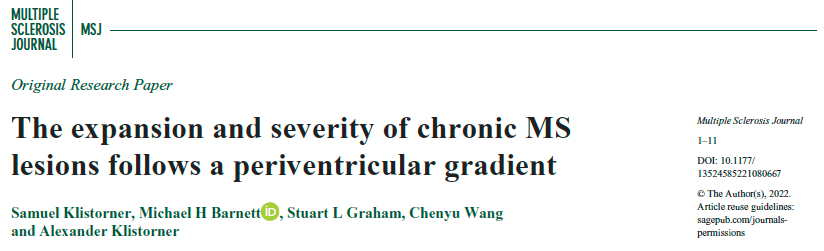
Novel Technical Advances:
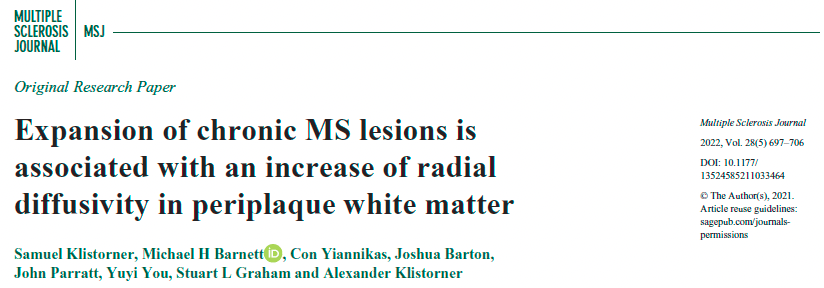
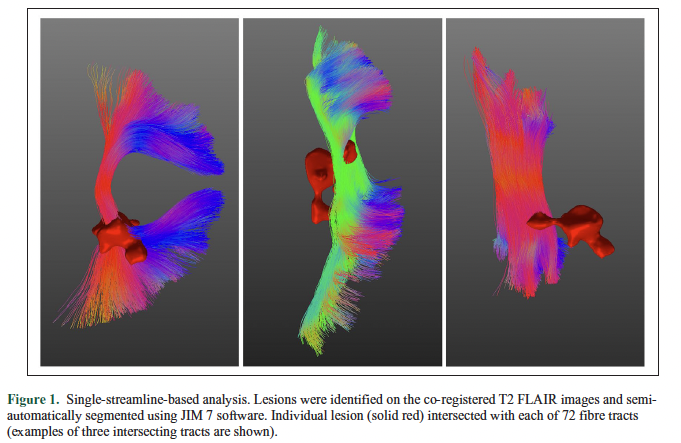
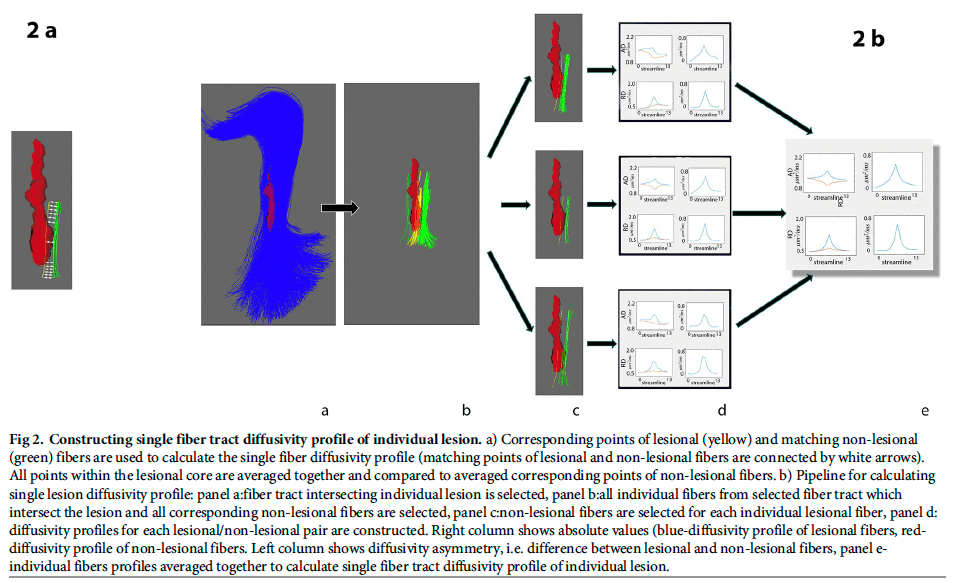
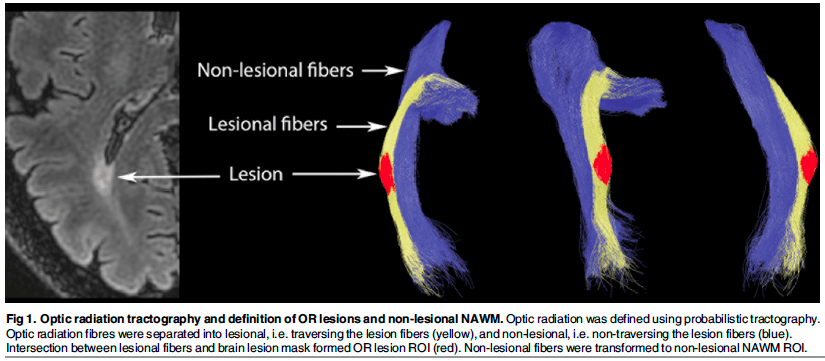
- Used advanced diffusion tensor imaging to track microstructural changes over time
- Developed methods to precisely analyze lesion cores separate from edges
- Created techniques to account for brain atrophy when measuring lesion changes
- Established ways to quantify progressive tissue damage in stable lesions
Clinical Implications:
- Explains why current MS treatments may not fully prevent disease progression
- Suggests need for additional therapeutic approaches targeting chronic lesion damage
- Highlights importance of considering gender differences in clinical trials
- Demonstrates value of monitoring lesion changes to predict disease course
Why It Matters:
Understanding how chronic lesions continue to cause tissue damage even without new inflammation provides crucial insights into MS progression. The findings suggest that protecting demyelinated axons and promoting remyelination may be critical therapeutic goals, alongside current anti-inflammatory treatments.